Common Keratoconus Questions
What is keratoconus?
Keratoconus is a degenerative eye disease that causes the cornea to thin and bulge, creating a cone-like irregular shape. Because the cornea is responsible for refracting most of the light that comes into the eye, any irregularity of the cornea can result in significant visual impairment. Keratoconus most often appears in a person’s late teenage years; although it has been diagnosed in people in their forties and fifties. The eye disease has been estimated to occur in roughly one out of every 2,000 people in the general population. No significant geographical, gender, ethnic, or social pattern has been established, and keratoconus occurs in all parts of the world.
What causes keratoconus?
The exact cause of keratoconus is not known; however, there are many theories on what may trigger this disease. It is important to note that no one theory provides a complete explanation, and it is likely that keratoconus is caused by a combination of things. It is believed that genetics, the environment, and the endocrine system all play a role in keratoconus:
Genetic Causes:
One scientific view is that keratoconus is developmental (i.e., genetic) in origin because in some cases there does appear to be a familial association. From the presently available information, there is less than a one in ten chance that a blood relative of a keratoconic patient will have keratoconus. The majority of patients with keratoconus do not have other family members with the disease. Some studies show that keratoconus corneas lack important anchoring fibrils that structurally stabilize the anterior cornea. This increased flexibility allows that cornea to “bulge forward” into a cone-shaped appearance.
Eye Rubbing:
Keratoconus corneas are more easily damaged by minor trauma such as eye rubbing. Poorly fit contact lenses (that rub against the irregularity of the KC cornea) have been suggested as a possible cause of keratoconus; this has not been proven and remains questionable.
Allergies:
Many who have keratoconus report vigorous eye rubbing and also have allergies (which cause eye itching and irritation, leading to eye rubbing), however, the link to allergic disease also remains unclear.A higher percent of keratoconic patients have the atopic disease than the general population. Disorders such as hay fever, eczema, asthma, and food allergies are all considered atopic diseases. Those with KC are advised to avoid eye rubbing as much as possible.
Oxidative Stress:
Some studies indicate an abnormal processing of the superoxide radicals in thekeratoconus cornea and an involvement of oxidative stress in the pathogenesis of this disease. Keratoconus corneas lack the ability to self-repair routine damage easily repaired by normal corneas. Like any tissues in the body, the cornea creates harmful byproducts of cell metabolism called free radicals. Normal corneas, like any other body tissue, have a defense system in place to neutralize these free radicals so they don’tdamage the collagen, the structural part of the cornea, weakening it and causing the cornea to thin and bulge. The keratoconus corneas do not possess the ability to eliminate the free radicals so they stay in the tissue and can cause structural damage.
Hormonal Causes:
Another hypothesis is that the endocrine system may be involved because keratoconus is generally first detected at puberty and progresses during pregnancy. This theory is still controversial and has not been proven.
Environmental Factors:
Keratoconus may also be associated with overexposure to ultraviolet rays from the sun, excessive eye rubbing, a history of poorly fit contact lenses and chronic eye irritation.
Endocrine System:
Another hypothesis is that the endocrine system (which dictates the release of hormones) may be involved, since keratoconus is often first diagnosed in adolescence.
What are the symptoms of keratoconus?
Blurred and distorted vision and frequent eyeglass prescription changes are the first signs of keratoconus. However, blurred and distorted vision occurs as a result of many other types of eye disease, so it is important to visit an experienced eye care professional for diagnosis immediately when noticing any changes in vision. Typically keratoconus occurs in both eyes with one eye more severe than the other. Additional symptoms of keratoconus include:
- Increased light sensitivity
- Difficulty driving at night
- Halo’s and ghosting (especially at night)
- Eye strain
- Headaches and general eye pain
- Eye irritation and excessive eye rubbing
How is keratoconus treated?
Keratoconus is primarily treated with contact lenses because glasses cannot to visually correct the irregular form of the cornea. Surgical treatment options are also available and are typically used when contact lens wear is no longer possible.
Contact Lens Treatment Options
Hybrid Contact Lenses
Hybrid contact lenses are the latest and most advanced option available in contact lenses specifically designed for keratoconus and irregular cornea patients. Using a revolutionary technology, hybrids combine the best of both worlds – the crisp vision of a high-oxygen rigid gas permeable (RGP) contact lens with the all-day comfort and convenience of a soft lens. Hybrids are specifically designed to restore vision to patients with the many types and stages of keratoconus. Because the lens design vaults over the cornea, there’s minimal risk of corneal scarring, making hybrid lenses a healthy treatment option for keratoconus. In addition, the soft skirt of the hybrid design helps to center the contact lens over the visual axis regardless of where the cone is located on the cornea or how large it is, thereby decreasing visual distortions and providing superior vision. The hybrid design also prevents dirt from getting under the lens and will not pop out unexpectedly. No other contact lens available today can provide all of these benefits in a single product.
What is a hybrid contact lens?
Hybrid contact lenses are an advanced contact lens option specifically designed for keratoconus and irregular cornea patients. The center of the lens is an RGP and it is surrounded by a soft lens material. Previously there were only two choices in contact lenses? “Hard” (RGP) lenses provided a GOOD vision but were often irritating and uncomfortable. Soft lenses offered GOOD comfort, but couldn’t correct your vision problems. Now, a technological breakthrough makes having to compromise a thing of the past. Hybrid contact lenses offer all the benefits of RGP and soft contact lenses without any of the disadvantages of an overall GREAT contact lens experience. Using a revolutionary technology, hybrids combine the best of both worlds – the crisp vision of a high-oxygen rigid gas permeable (RGP) contact lens with the all-day comfort and convenience of a soft lens. Hybrids are specifically designed to restore vision to patients with the many types and stages of keratoconus. Because the lens design vaults over the cornea, there’s minimal risk of corneal scarring, making hybrid lenses a healthy treatment option for keratoconus. In addition, the soft skirt of the hybrid design centers the contact lens more closely over the visual axis regardless of where the cone is located on the cornea or how large it is, decreasing visual distortions and providing superior vision. The hybrid design also prevents dirt from getting under the lens and will not pop out. No other contact lens available today can provide all of these benefits in a single product.
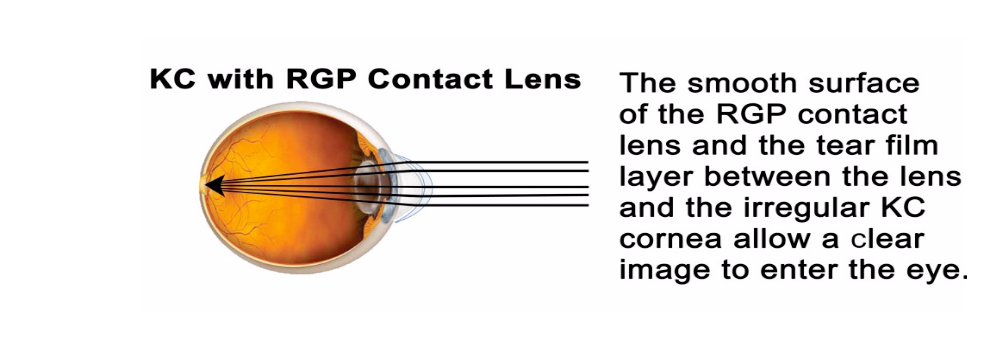
Rigid Gas Permeable (GSP) Lenses
RGP lenses are made from a rigid material that does not drape over the irregularly shaped cornea, but rather, holds its shape and creates a layer of tears between the cornea and the back surface of the lens. This tear layer neutralizes the irregular shape of the cornea. Consequently, RGPs provide better vision than soft lenses. Unfortunately, for those with keratoconus, RGPs may not provide adequate vision correction. This is because RGP lenses tend to migrate toward the location of the cone, which is usually not on the visual axis, which is near the center of the cornea. For this reason, patients who wear RGPs typically experience problems with inconsistent vision. Furthermore, RGPs are often uncomfortable, inconvenient, allow dirt to be trapped under the lens and may pop out. They can also lead to corneal scarring because they are commonly designed to fit touching the surface of the cone.
Scleral Lenses
Scleral lenses are very large RGP lenses that can provide an adequate vision but often require very precise and skilled fitting by your eye care professional. Sclerals occasionally have to be removed and reinserted with fresh saline during the day to keep your vision clear and comfortable.A scleral lens, also known as a scleral contact lens and ocular surface prostheses is a large contact lens that rests on the sclera and creates a tear-filled vault over the cornea. Scleral lenses are designed to treat a variety of eye conditions, many of which do not respond to other forms of treatment.
NovaKone Soft Contact Lenses
Custom soft lenses for keratoconus offer a new approach to keratoconus vision correction. Alden Optical’s new NovaKone™ lens offers a high level of comfort and excellent vision. While NovaKone lenses can be a viable solution for all stages of keratoconus (KC) and pellucid marginal degeneration (PMD), they’re especially effective for patients with more advanced conditions and for those who have failed to tolerate other lenses. NovaKone offers extraordinary comfort and can be an excellent adjunct to other forms of correction.
Soft Contact Lenses
Soft contact lenses are comfortable but are usually unable to visually normalize the irregularities of the keratoconic cornea and therefore do not provide acceptable vision. Soft lenses drape over the irregular corneal surface causing the surface of the lens to assume the same irregular shape as the cornea. This abnormal shape is the reason for blurred and distorted vision. As the cornea becomes more irregular, soft lenses become less effective.
Piggyback Lenses
“Piggyback” lenses are RGP’s and soft lenses that are worn at the same time. In some cases, this approach may be more successful than soft or RGP lenses alone, but because of the complexities of handling and care, possible eye health problems due to the decrease in oxygen able to move to the cornea through both lenses, and difficulty with lens centration, success rates are marginal.

Surgical Treatment Options
Patients with keratoconus often ask “Can I have surgery to correct my keratoconus?” There are surgical
options that are designed to strengthen, reshape or replace the irregular surface of a keratoconic cornea, and
perhaps lessen the impact of keratoconus, but unfortunately none will reverse the progression that has taken
place.
The most common surgical treatment options for keratoconus are Intacs®, corneal collagen crosslinking,
corneal transplant or some combination of these procedures.
Intacs®
Intacs are semi-circular plastic implants that are inserted into the middle of the cornea. The intent is to reshape the cornea to a more normal shape to improve vision. Commonly Intacs do not leave the cornea completely regular in shape, and contacts are still needed for further correction. Intacs are used to improve the patient’s vision, and possibly delay or eliminate the need for a corneal transplant.
 Corneal Collagen Cross-linking (CXL)
Corneal Collagen Cross-linking (CXL)
A new treatment option called corneal collagen cross-linking (CXL) is currently undergoing FDA clinical trials in the United States to determine its safety. With the corneal cross-linking procedure, custom-made riboflavin drops saturate the cornea, which is then activated by ultraviolet-A light. This process has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking and strengthen the cornea.

Corneal Transplant
A corneal transplant is a surgery in which a plug of approximately 7.5mm–including the steepest, most irregular part of the cornea–is removed and replaced with corneal tissue from a donor's eye. The transplanted tissue is then sutured into place. Lamellar Keratoplasty is a relatively new technique which involves the removal of only a partial thickness of the cornea. The theoretical advantage is a lower risk of rejection because the major target for corneal rejection is not transplanted. The resulting cornea is generally flatter and smoother than before, but most often there are still irregularities that are best corrected by a contact lens.
Is it common for KC patients to wear different type lenses in each eye?
Most experienced contact lens fitters try to maintain symmetry with similar lenses in both eyes. This usually simplifies lens care and can avoid a few other potential issues. However, keratoconus fitting can be challenging making two different lenses essential to obtain an ideal fit. I wouldn’t worry about having different lenses brands or even types in each eye, but if it concerns you, just ask your contact lens specialist to explain why they chose that approach.
Has there been any research into using the patient's own stem cells to create a new cornea?
As many of you know stem cell research and efforts to develop a replacement cornea have both been ongoing for many years. While progress has been made, we are still a few years away from any practical applications.
Can keratoconus affect a person's balance?
Balance depends upon input from the inner ear and the visual system. That information is processed by the brain to help orient us in space. Anything that disturbs inner ear function or vision can disrupt the balance. Likewise, neurological problems can also cause imbalance.If you are having balance issues caused by your visual system, they may be due to visual or prescription differences between your two eyes that your doctor may be able to easily correct. Sometimes it may be due to a prescription that has changed. Because balance problems can have other causes – some potentially serious, you should discuss this with your doctor at your next visit or sooner if it worsens.
Since I've been wearing the RPG contacts my eyes get very red, I use drops to get rid of the redness but then it comes back. Is this normal?
First, discontinue the drops. Eye drops for redness usually contain vasoconstrictors (medicine that makes the blood vessels smaller). Over time, the vasoconstrictors become irritating which causes more redness. This sets up a vicious cycle causing some patients to become virtually addicted to these drops. Using preservative-free artificial tears can help make the eyes feel more comfortable and do not contain these vasoconstrictor medicines.
That said, redness in a GP lens wearer is often a sign of a lens fitting problem or drying of the ocular surface related to the lens fit. Fitting issues can easily be identified by your contact lens specialist. Sometimes a minor change in fit, polishing the lens surface, a new material or a new lens care solution may solve the problem. Occasionally, eliminating redness can be challenging. Other issues should be explored for a persistent red eye in a lens wearer. These include underlying dry eye and allergy. All in all, it is best to discuss this with your contact lens fitter who can find the cause and help solve the problem.
I was supposed to have Lasik surgery, however, the doctor who was to perform the surgery said that because my mother had KC that there is a slight chance that laser surgery might cause keratoconus even though my eyes are healthy. Is that true?
Keratoconus has a genetic basis. Having a parent who has the disorder may increase your risk of developing keratoconus or of developing corneal thinning post-LASIK. You may also have subclinical evidence of keratoconus that has concerned your doctor. You should ask if his recommendation is based solely on your family history or if there are other factors like abnormal corneal topography. Ultimately, you have to decide if the risk is justified. Sometimes a second opinion is helpful. My advice is when it comes to your sight; it is better to err on the side of caution.
Does high pressure cause the thinning cornea to bulge?
A certain amount of internal pressure is normal. Normal pressure is a factor in maintaining the shape of your eye whether you have keratoconus or not. High pressure can be indicative of glaucoma but isn’t necessarily related to keratoconus.
Is Keratoconus always degenerative, or is it possible for it to stay at a mild level?
Keratoconus is a highly variable and unpredictable disease. Many patients have a mild form and do not progress significantly. However, there is no way to predict this for an individual.
Do most people have the condition in both eyes? If you do have it in one eye only, does that mean you might develop it in the other eye at some point? Is certain that you will? When will you know that you are in the clear?
Most experts believe that keratoconus is always bilateral – that is that it always affects both eyes. However, because of variability, the condition may be so mild in one eye that it is virtually undetectable. It may stay that way or the better eye may progress over time. Unfortunately, there is no way to know which will occur.
I have noticed a daily aching pain in my right eye that also hurts when I blink or move my eye when my eyelid is closed. Is this normal for KC?
You are not alone. Many keratoconus patients complain of discomfort or outright pain. Since pain may also be a sign of other problems you should bring this to your doctor’s attention as soon as possible.
Is it common for people with keratoconus to feel more tired or require more sleep because their eyes are under more strain while they are awake?
Although this isn’t a common symptom, visual strain can be tiring and can lead to fatigue. Here too, I would discuss this with your doctor to ensure that your correction is appropriate and that nothing else is amiss.




